Open Access, Volume 9
Coronary cameral fistula connecting right coronary artery to left ventricle – A case report
Satyanarayana R Yaramala1*; Virupaxi V Hattiholi1; Richard Saldana2; Pooja M Kavatagimath2
1Department of Radio-diagnosis, Jawaharlal Nehru Medical College, Belgaum, Karnataka, India.
2Department of Cardiac Surgery, Jawaharlal Nehru Medical College, Belgaum, Karnataka, India.
Satyanarayana R Yaramala
Department of Radio-diagnosis, Jawaharlal Nehru Medical College, Belgaum, Karnataka, India.
Email: yaramala89@gmail.com
Received : February 11, 2023
Accepted : March 28, 2023
Published : March 31, 2023,
Archived : www.jclinmedcasereports.com
Abstract
A Coronary Cameral Fistula (CCF) is a congenital or acquired abnormal vascular communication of coronary arteries with any of the cardiac chambers. The prevalence of CCF in adult patients was low (0.09 – 0.5%) and only 3-5% of all CCF drains into the left ventricle. In this report, we are presenting a rare case of incidentally detected coronary cameral fistula communicating the right coronary artery with the left ventricle in an ischemic patient due to double vessel disease.
Keywords: Coronary cameral fistula; Right coronary artery; Left ventricle.
Abbreviations: CCF: Coronary Cameral Fistula; CAFs: Coronary Artery Fistulas; LAD: Left Anterior Descending Artery; LCX: Left Circumflex Artery; RCA: Right Coronary Artery; PLV: Posterior Left Ventricular.
Copy right Statement: Content published in the journal follows Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0). © Yaramala SR (2023)
Journal: Open Journal of Clinical and Medical Case Reports is an international, open access, peer reviewed Journal mainly focused exclusively on the medical and clinical case reports.
Citation: Yaramala SR, Hattiholi VV, Saldana R, Kavatagimath PM. Coronary Cameral Fistula Connecting Right Coronary Artery to Left Ventricle – A Case Report. Open J Clin Med Case Rep. 2023; 2004.
Introduction
Coronary artery fistulas are abnormal vascular communications in which blood is shunted bypassing the myocardial capillary network into the cardiac chambers or any segment of systemic or pulmonary circulation affecting hemodynamic parameters [1]. Coronary cameral fistula (CCF) detected in adulthood is associated with an increased risk of heart failure, myocardial ischemia, infective endocarditis, arrhythmias, rupture, and even sudden cardiac death [2].
Case Report
A 57 year old female patient with a history of hypertension and diabetes mellitus presented to the cardiology outpatient clinic of our hospital with giddiness and angina chest pain for 15 days. The cardiac and respiratory exam was unremarkable. ECG showed normal sinus rhythm with no ST/T wave changes. The exercise treadmill test was positive. Echocardiography showed Grade-1 diastolic dysfunction. Catheter angiography shows a lesion involving mid LAD and mid LCX causing 80% narrowing with right dominant circulation and tortuous proximal RCA draining into the left ventricle via PLV branches. Further referred to the radiology department for a preoperative detailed evaluation of coronary cameral fistula. CECT showed dilated, tortuous proximal right coronary artery with good flow seen coursing along the inferior atrioventricular groove and posterior left ventricular branches draining as coronary cameral fistula to the left ventricle. Three-dimensional volume-rendered images accurately depicted the origin and course of CCF.
The patient successfully underwent coronary cameral fistulectomy and came for postoperative CECT evaluation. Post-operative CECT showed the right main coronary artery (RCA) arising from the right sinus of Valsalva coursing towards the right side and abruptly ending in the mediastinum, one reversed saphenous vein graft (Rt RSVG) arising from the ascending aorta on right side coursing inferiorly and anastomosed to PDA. Another reversed saphenous vein graft (Lt RSVG) arising from the ascending aorta on the left side is anastomosed to the distal-most portion of a left anterior descending artery. There is non-visualization of the residual fistulous tract between the RCA and left ventricular chamber owing to the successful repair of the coronary cameral fistula.
Imaging Findings
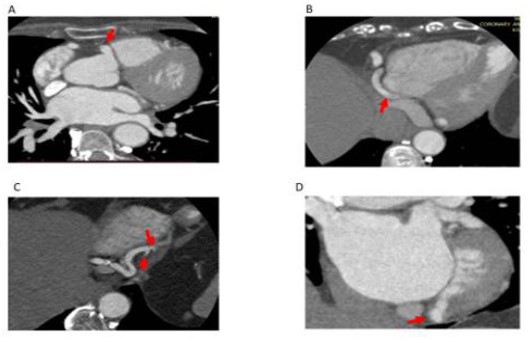
Coronary cameral fistula in a 57-year-old female patient presented with chest pain. (a) Axial CT coronary angiogram images show a right coronary artery originating from the right sinus of Valsalva (arrow in a) coursing into the atrioventricular groove (arrow in b) with a subsequent bifurcation forming the posterior descending artery (PDA) (curved arrow in c) and Posterior Left Ventricular branch (PLV) (arrow in c). PLV is draining as coronary cameral fistula into the left ventricle chamber (arrow in d).
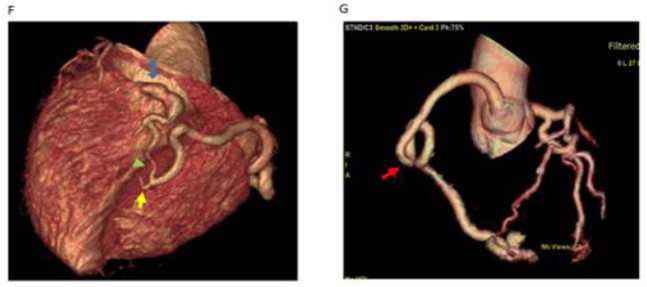
Coronary cameral fistula in a 57-year-old female patient presented with chest pain. Volume-rendered CT images obtained at different levels show a right coronary artery coursing in the atrioventricular groove with a subsequent bifurcation forming the posterior descending artery (PDA) (yellow arrow in f) and posterior left ventricular branch (PLV) (green arrow in f). PLV is draining as coronary cameral fistula into the left ventricle chamber (blue arrow in f). Note the tortuous course of the proximal segment of the right coronary artery (arrows in g).
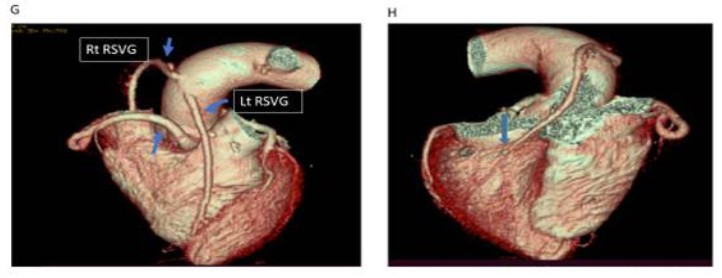
Coronary cameral fistula in a 57year old female patient who subsequently underwent surgical repair. Post-procedural axial (a, b, c, d, e & f)) CT coronary angiogram images show a right coronary artery arising from the right sinus of Valsalva (arrow in a) coursing towards the right side and abruptly ending in the mediastinum, coronal view (b) shows the right coronary artery stump closed with vein patch (arrow in b) in the mediastinum. Note one reversed saphenous vein graft arising from the ascending aorta on the right side (straight arrow in c) coursing inferiorly (arrow in d) and anastomosed to PDA (arrow in e). Note there is no visualization of the residual fistulous tract between the RCA and left ventricular chamber (arrow in f) owing to the successful repair of the coronary cameral fistula.
Post-procedural volume-rendered (G &H) CT images show a right main coronary artery (RCA) (plain blue arrow in G), one reversed saphenous vein graft (Rt RSVG) arising from the ascending aorta on the right side (G) coursing inferiorly and anastomosed to PDA (arrow in H). Another reversed saphenous vein graft (Lt RSVG) arising from the ascending aorta on the left side (G) anastomosed to a distal-most portion of the left anterior descending artery (not shown here). Note there is no visualization of the residual fistulous tract (H) between the RCA and left ventricular chamber owing to the successful repair of the coronary cameral fistula.
Discussion
Coronary artery anomalies are rarely occurring in 1% of the population. Anomalies are categorized based on the origin, course, and termination of coronary arteries, and coronary fistulas are categorized under abnormalities in termination. Coronary artery fistulas (CAFs) are abnormal communications in which blood is shunted bypassing the myocardial capillary network into the cardiac chambers and systemic or pulmonary circulation. The estimated prevalence of CAFs is 0.02% in the general population, CAFs constitute 0.2%-0.4% of congenital cardiac anomalies, and no race or sex predilection [3]. The name Coronary Cameral Fistula (CCF) specifically represents coronary artery fistula between a coronary artery and any of the cardiac chambers. Depending upon the type of communication with the cardiac chamber classified as arterio-luminal or arteriosinusoidal (communication through a sinusoidal network rather than direct communication) [4].
The prevalence of CCF in adult patients was low (0.09 – 0.5 %). More than 90% of CCF are congenital or sporadic. Acquired coronary artery fistulas result from iatrogenic events such as coronary artery stent placement, coronary artery bypass grafting, trauma, and chest irradiation. CCF can be single or multiple, most commonly CCF originates from the right coronary artery (55%), and the most commonly involved chamber is the right ventricle (41%) followed by the right atrium (26%), and left atrium and left ventricle (3%-5%) [5].
Historically invasive coronary angiography was used to evaluate the coronary artery fistulas, with good temporal resolution now ECG-gated CT coronary angiogram is considered as a test of choice for pre and post-operative evaluation of coronary cameral fistulas [6]. Cardiac CT is very useful to diagnose particularly when there is ischemia due to coronary atherosclerosis.
As described in the literature management of CAFs is surgical closure for the arterioluminal subtype and the arteriosinusoidal subtype is managed with beta-blockers as these are less amenable for surgery. Indications for invasive treatment include significant hemodynamic compromise due to shunting, myocardial ischemia, or congestive cardiac failure. However, there is a risk of myocardial infarction or recurrence of fistula postoperatively. Incidentally detected asymptomatic patients are conservatively managed with serial follow-ups [7].
References
- Angelini P, Villason S, Chan AV, Diez JG. Normal and anomalous coronary arteries in humans. In: Angelini P, editor. Coronary artery anomalies: a comprehensive approach. Philadelphia: Lippincott Williams & Wilkins. 1999; 27-150.
- Yuksel S, Yasar E, Nar G, Gulel O, Demircan S, Yilmaz O, et al. Prevalence and characteristics of coronary-cameral communications in adult patients: Coronary angiographic analysis of 16,573 patients. Medical Principles and Practice. 2014; 23: 336-339.
- Maragkoudaki SS, Patrianako SA, Kallergi SE, Parthenaki SF, Varda SP. Case Report Case Report Echocardiographic Demonstration of Coronary Artery to Left Ventricle Fistulas: Case Report and Review of the Literature. 2014.
- Nagpal P, Khandelwal A, Saboo S, Garg G, Steigner M. Symptomatic coronary cameral fistula. 2015; 16: 65-67.
- Yun G, Nam TH, Chun EJ. Coronary artery fistulas: Pathophysiology, imaging findings, and management. Radiographics. 2018; 38: 688-703.
- Schmitt R, Froehner S, Brunn J, Wagner M, Brunner H, Cherevatyy O, et al. Congenital anomalies of the coronary arteries: imaging with contrast-enhanced, multidetector computed tomography. European radiology. 2005; 15: 1110-1221.
- Boyle S, Jesuthasan LSB, Jenkins C, Challa P, Ranjan S, Dahiya A. Coronary-Cameral Fistula. Circulation Cardiovascular imaging. 2019; 12: e008691.