Open Access, Volume 1
Use of the Perclose ProGlide Closure Device to Remove a Central Venous Catheter Inadvertently Inserted in the Right Subclavian Artery
Arturo Giordano , Nicola Corcione , Michele Polimeno , Stefano Messina , Giuseppe Biondi-Zoccai , Antonino G. M. Marullo3, Paolo Ferraro1,2
1Cardiovascular Interventions Unit, Pineta Grande Hospital, Castel Volturno, Italy
2Operative Unit of Hemodynamics, St. Lucia Hospital, San Giuseppe Vesuviano, Italy
3Department of Medical and Surgical Sciences and Biotechnologies, Sapienza University of Rome, Latina, Italy
4Eleonora Lorillard Spencer Cenci Foundation, Rome, Italy
Dr. Arturo Giordano
Cardiovascular Interventions Unit, Pineta Grande Hospital, Domiziana Street KM 30, 81030 Castel Volturno CE, Italy
Phone/Fax: +39-336-945902
Email: arturogiordano@tin.it
Received : January 31, 2015,
Accepted : March 30, 2015
Published : April 06, 2015,
Archived : www.jclinmedcasereports.com
Abstract
Central venous access is commonly adopted in sick patients requiring intensive management. The insertion and management of central venous catheters (CVC) in the subclavian vein is usually safe and feasible in experienced hands, but complications may occur, especially in subjects with anatomical variants or when CVC have to be deployed in a hurry. An uncommon but potentially serious complication is the deployment of a CVC in the subclavian artery, as removal and hemostasis may prove challenging given the deep seating of the arteriotomy. We hereby report the case of a patient in whom a CVC had been inadvertently deployed in the right subclavian artery. Given the many comorbidities, a minimally invasive removal and hemostasis approach was attempted, using a Perclose ProGlide to seal the arteriotomy and concomitant intravascular balloon occlusion to ensure complete and timely hemostasis. This clinical vignette highlights the importance of mastering different skills and combining different devices to ensure the optimal management of vascular complications.
Keywords: gastrointestinal metastases; invasive lobular breast carcinoma; pathohistological analysis; immunohistochemical analysis; complex treatment.
Copy right Statement: Content published in the journal follows Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0). © Giordano A et al
Journal: Open Journal of Clinical and Medical Case Reports is an international, open access, peer reviewed Journal mainly focused exclusively on the medical and clinical case reports.
Citation: Giordano et al. Use of the perclose proGlide closure device to remove a central venous catheter inadvertently inserted in the right subclavian artery. Open J Clin Med Case Rep. 2015; 1001
Introduction
Improved life expectancy and reined means for intensive care have lead to an exponential increase in the number of patients receiving central venous catheters (CVC) for diagnostic or therapeutic purposes. The typical access sites for CVC are the internal jugular and subclavian veins, with the subclavian vein being considered safer for long-term CVC use, but requiring more technical skills for successful puncture. Indeed, the complications of subclavian vein access may include hematoma, pneumothorax, hemothorax, nerve injury, and arterio-venous istula.(1) Another complication is the inadvertent deployment of the CVC in the subclavian artery. This occurrence may lead to life-threatening complications if drugs with potential for limb injury are administered. Even if this is not the case, removal of a CVC from a subclavian artery may prove challenging if open surgical repair is contraindicated in light of patient comorbidities, given the deep seating of this vessel and the complex anatomical relationship between this vessel and the lung, the clavicle, and the ribs. When a CVC has been inadvertently deployed in the subclavian artery, use of a vascular closure device may lead to successful and safe hemostasis, as long as the risk of failure is minimized or its potential consequences amended.(2-3) We hereby report a case of successful use of the Perclose ProGlide suture-based vascular closure device (Abbott Vascular, Santa Clara, CA, USA) to remove a central venous catheter inadvertently inserted in the right subclavian artery, with concomitant vessel protection with an intravascular balloon.
Case Presentation
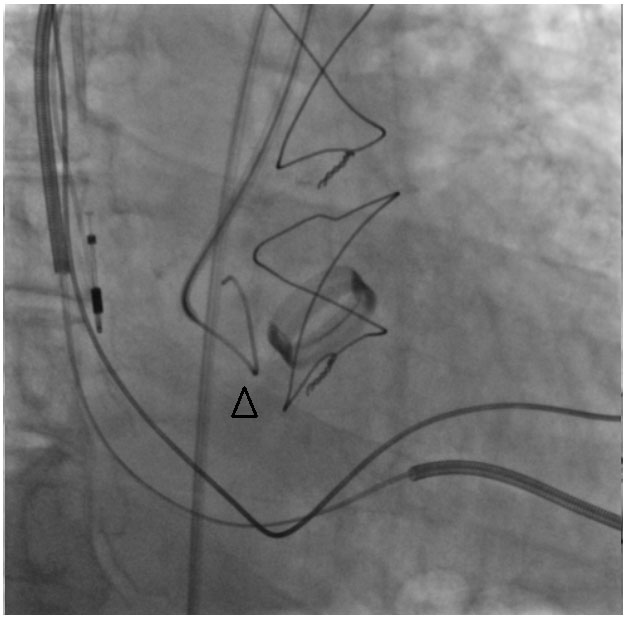
A 70-year-old gentleman was referred to our institution after having received a CVC for the management of acute pulmonary edema and suspected endocarditis, as soon as the referring physician recognized that the CVC had not been deployed in the right subclavian vein, as intended, but inadvertently in the right subclavian artery (Figure 1).
His medical history was notable for arterial hypertension and family history of coronary artery disease. He had also undergone surgical aortic valve replacement for severe aortic stenosis when he was 50 years old, with a Bicarbon 23 valve (Sorin, Saluggia, Italy). Given a subsequent worsening in left ventricular systolic function and widening of the QRS, he had then been implanted with an automated implantable cardioverter deibrillator/cardiac resynchronization therapy (AICD/CRT) device. Despite this, he had suffered from several bouts of sustained ventricular tachycardia, requiring in the years preceding the index admission three separate left ventricular ablation procedures. A few days before being transferred to our institution he had suffered from severe shortness of breath, requiring hospital admission in another hospital. During such admission, a diagnosis of acute pulmonary edema and suspected endocarditis had been made, and an attempt to deploy a CVC in the right subclavian vein had been made. However, pressure readings from the deployed CVC had shown that the right subclavian artery had been punctured instead. After deploying, this time correctly, another CVC in the right jugular vein, the patient was referred to us for the removal of the CVC.
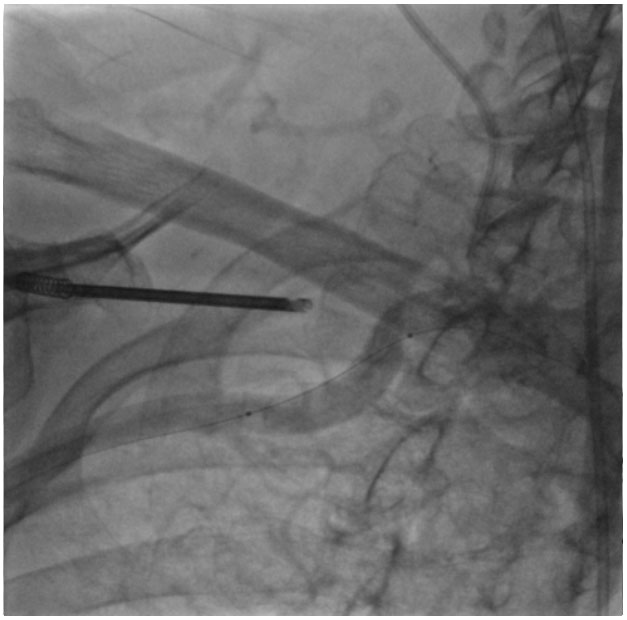
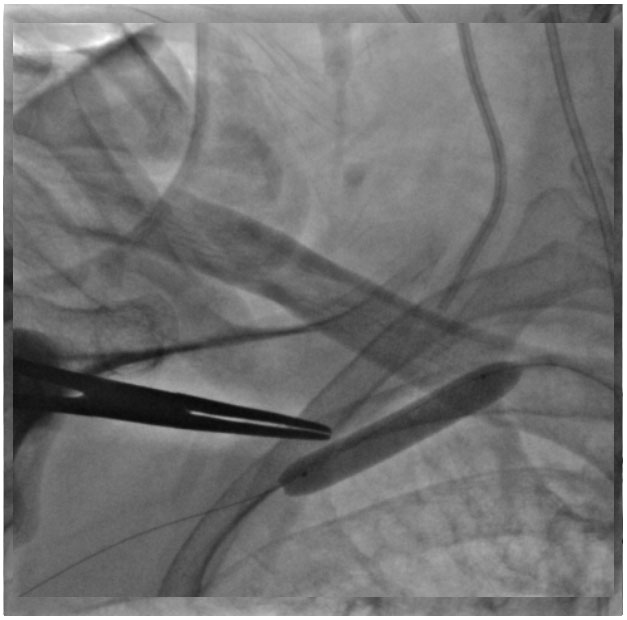
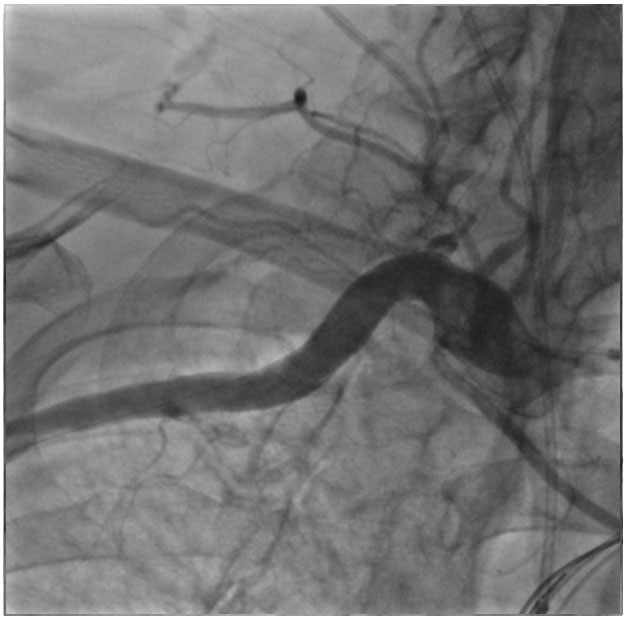
In light of the patient comorbidities and our extensive experience with the management of challenging vascular access sites, we opted for a minimally invasive approach. We accessed the right femoral artery with a short 6 French sheath. Then, we performed selective angiography of the right subclavian artery and deployed a 0.018" Emerald guidewire (Cordis, Miami Lakes, FL, USA), with subsequent deployment over such guidewire of a 7.0x40 mm Senri balloon (Terumo, Tokyo, Japan). Keeping the balloon uninlated to avoid entanglements, we deployed over a 0.035" Emerald guidewire (Cordis) a Perclose ProGlide 6 French suture-mediated closure system. After knot pushing and suture trimming with the proprietary accessory, further knot pushing was performed with a straight Kocher hemostat, concomitantly inlating inside the right subclavian artery the Senri balloon at 16 atmospheres for 5 minutes. After removal of the straight Kocher hemostat and balloon delation, the inal angiographic control disclosed adequate hemostasis, without any hematoma at skin inspection. The patient was then admitted to the stepdown medical care unit with an uneventful subsequent clinical stay.
Discussion
The exponential uptake of means for intravascular access has increased the treatment opportunities in intensively cared patients, but has also increased the risk of complications or untoward adverse events.(1) An uncommon but dificult to manage complication is represented by the inadvertent puncture and deployment of the CVC into an arterial rather than a venous vessel. While surgical repair can always be envisioned in such cases, it may be associated with additional complications, especially in subjects with severe or multiple comorbidities.
The use of vascular closure devices has improved the management of diagnostic and therapeutic procedures requiring arterial access, by providing a safe and time-saving means to achieve hemostasis even in the context of ongoing anticoagulation.(4) Indeed, vascular closure devices appear particularly promising to manage large bore arteriotomies, or arterial access in sites which may be challenging to reach surgically.(5-6) Accordingly, the use of vascular closure device to enable safe and effective removal of a CVC which has been inadvertently deployed in an artery has been already proposed in a number of reports.(2-3)
We hereby expand the evidence base on this topic highlighting the promising role of the Perclose ProGlide suture-based closure device for a CVC which has been inadvertently deployed in the right subclavian artery, especially when combined with a simultaneous additional arterial access for bail-out purposes and for temporary intravascular balloon occlusion. Indeed, an updated analysis of the evidence base on this topic highlights several dozens of case reports are available on vascular closure device implantation for willing or inadvertent subclavian artery access, though most focus on the Angio-Seal collagen-plug device (St. Jude Medical, Saint Paul, MN, USA), and only a few on the Perclose ProGlide. While operators experienced with subclavian access and vascular closure devices might think this is not a novel case, most operators are not experienced in subclavian access, in vascular closure devices, and in their combination. Accordingly, our case may represent an incrementally useful addition to the current body of data on vascular closure devices for subclavian artery access. In light of our extensive experience with the Perclose ProGlide for transfemoral aortic valve replacement (TAVR), we chose this speciic device in this scenario, but other devices could have been envisioned.(7-8) Yet, using collagen-plug devices such as Angio-Seal or Exoseal (Cordis), could lead to a potential risk of cerebral embolization in this speciic setting, potentially contraindicating their selection.
In conclusion, the Perclose ProGlide suture-based vascular closure device can be successfully used to remove a central venous catheter inadvertently inserted in the right subclavian artery, especially when combined with concomitant vessel protection with an intravascular balloon.
Figures
Figure 1. Use of the Perclose ProGlide closure device to remove a central venous catheter inadvertently inserted in the right subclavian artery.
References
- Bowdle A. Vascular complications of central venous catheter placement: evidence-based methods for prevention and treatment. J Cardiothorac Vasc Anesth. 2014; 28: 358-368.
- Berlet MH, Steffen D, Shaughness G, Hanner J. Closure using a surgical closure device of inadvertent subclavian artery punctures during central venous catheter placement. Cardiovasc Intervent Radiol. 2001; 24: 122-124.
- Meyhoefer J, Lehmann H, Minden HH, Butter C. Closure of the subclavian artery puncture site with a percutaneous suture device after removal of an arterial pacemaker lead. Europace. 2006; 8: 1070- 1072.
- Byrne RA, Cassese S, Linhardt M, Kastrati A. Vascular access and closure in coronary angiography and percutaneous intervention. Nat Rev Cardiol. 2013; 10: 27-40.
- Kim TH, Shim WH. Postclose technique for large sheath arterial access using perclose(TM) in emergency endovascular repair. Catheter Cardiovasc Interv. 2014; 83: 1176-1179.
- Schäfer U, Ho Y, Frerker C, Schewel D, Sanchez-Quintana D, Schofer J, Bijuklic K, Meincke F, Thielsen T, Kreidel F, Kuck KH. Direct percutaneous access technique for transaxillary transcatheter aortic valve implantation: "the Hamburg Sankt Georg approach". JACC Cardiovasc Interv. 2012; 5: 477-486.
- Biondi-Zoccai GG, Fusaro M, Tashani A, Mollichelli N, Medda M, De Giacobbi G, et al. Angioseal use after antegrade femoral arteriotomy in patients undergoing percutaneous revascularization for critical limb ischemia: a case series. Int J Cardiol. 2007; 118: 398-399.
- Biondi-Zoccai G, Peruzzi M, Frati G. Use of the 8-f angio-seal vascular closure device for much larger sheaths: successfully itting a square PEG into a round hole? J Endovasc Ther. 2012; 19: 501-503.